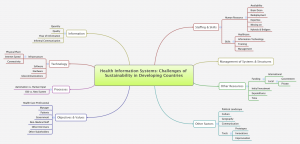
#HI201 #MSMHI week 4 Task: Mindmap of Challenges of Sustainability of Health Information Systems in Developing Countries
Bridging the Gap and Avoiding Collisions
Heeks (1) design-reality gap model quite simplistically, summarised challenges of sustainability of health information systems along seven dimensions: (1) information, (2) technology, (3) processes, (4) objectives and values, (5) staffing and skills, (6) management systems and structures, and (7) other resources. To succeed, HIS design and concepts should be as close to how these factors are in the real world.
Information processed by HIS should be of sufficient quantity, of good quality, and flows well from data collection to processing and analysis. If the design does not meet the data requirements on the field, HIS is bound to fail. HIS should also take into consideration the wealth of informal communication that may influence any HIS.
Technology encompasses infrastructure, software development, hardware, and even telecommunications equipment. For the HIS design to work, all these should be considered before implementation on ground zero.
Processes that require automation cannot dissociate completely from those requiring human input. An old system that has worked and is efficient, cannot just be replaced by an unproven novel system, and worse, by one that cannot exceed the efficiency of the old system. If the comparison is status quo, it will tilt the balance towards retention of old ways. Novel procedures and processes will not be accepted.
Objectives and Values should be defined by different stakeholders–the healthcare professional, the health facility manager, the patient, researchers, non medical personnel, the government (department of health) may all have different objectives that may not always be in perfect unison and may clash despite a common goal. Different perceptions of reality, variations in objectives and values affect the clinical utility of an HIS. As such, the developer and designer should not just make assumptions, but rather consult all possible stakeholders and end-users before undertaking an HIS that will be attuned to the needs of all, if not that of the greater majority. A tough feat!
Staffing and Skills. Human resources remain wanting for HIS. The task is daunting, and the personnel too few. When available and trained well, they may get lured by brain drain, redeployment and find themselves “moving on” to another task. Not only should there be warm bodies, they have to be skilled in both healthcare and information technology, and involve themselves in training for the HIS to be accepted and for HIS to work efficiently. To bridge the gap, hybrids (e.g., health personnel trained in information technology) or “bridgers” who coordinate with different stakeholders should be around to modify, innovate and improvise.
Management System and Structures rarely have gaps but may still be susceptible to manipulation by human resources, opinion leaders, and decision makers.
Other resources especially in terms of time and funding also affect sustainibility. Implementation of an enormous task, such as the setting up of a health information system for a whole country requires the luxury of time. However, funding agencies, whether they are local or international would set finite time tables by which HIS are evaluated. In addition, after initial capital outlay or investment, there is continuing expenditure that should not deviate much from the initial budget proposed, and would requre that fund sources are available if not limitless. If this can be achieved, nirvana is within reach.
Other factors that this author would like to add are the country’s political landscape, our geography, and our culture. Politics affects bureaucratic red tape, the speed by which projects get approved, or receives a budget from government appropriation. Geography, as in the Philippines for example, the fact that we are an archipelago creates logistics and planning nightmare. The differences in culture, the fact that patients want to “see the physician eye to eye,” religious customs and rituals, all these affect implementation of an efficient information technology system attuned to health care delivery.
Communication systems also play a major role in starting, maintaining, as well as sustaining the success of any HIS. Internet speed is always an issue, as developing countries still grope for the optimal speed for the information superhighway. Tools for innovation, analysis and ability to compromise, modify, and improvise favour sustainability and success of an HIS. Communication lines between end-users, developers, and fund providers should be amicably intertwined and coexistent. Common goals and agenda can be set.
In summary, while the perfect fit is impossible, reducing the mismatch between actuality and design spells success and sustainability for any HIS anywhere.
References:
1. Heeks R. Health information systems: Failure, success and improvisation. Int J Med Informatics 2006; 75: 125-137.
2. Kimaro HC & Nhampossa JL. The challenge of sustainability of health information systems in developing countries: comparative case studies of Mozambique and Tanzania. J Health Informatics in Developing Countries 2007; 1 (1): 1-10.
Leave a Reply