Story of a COVID19 Survivor
Exposure
I was exposed last March 8, 2020. In a meeting, there were two who had recent travel to Malaysia. At that time, Malaysia was not in the list of “high risk” destinations, not until 2 days after our meeting. One of them was asymptomatic, the other rapidly deteriorated by the second week and was intubated. Thankfully, she has now pulled through and is on her way to full recovery. As many of us in that meeting (10 of 14) started having symptoms, 2 of whom believed it was “asthma,” for the rest it had to be COVID19. At that time, however, we did not qualify for testing, test kits were few, and we were just all on home quarantine. None of us who had symptoms were tested, except for the one severe case that was admitted.
My Symptoms
I had dry cough that was prolonged for about two weeks, had a one day malaise and tiredness, but had no sense of smell or taste for about a week, and a few sporadic episodes of diarrhea. I needed to be persistent, I was persistent. I was bothering and texting Dr. Karl Henson, every so often, and watched the Department of Health’s guidelines on testing almost daily. Finally, especially after our index case had deteriorated, I was finally told, that I could already be tested. My nasopharyngeal and oropharyngeal swabs were taken on day 11 from my onset of symptoms, or day 14 from my exposure. My real time-reverse transcription polymerase chain reactive (RT-PCR) test came back negative 3 days later.
Believe It or Not
Trained as a physician, I knew that not all tests were a 100% accurate. None of existing tests are a 100% sensitive. We base diagnosis and management on clinical history and presentation, more than just “treating a test result.” I felt I was a “false negative” — I was tested too late, or I had recovered by the time my swabs were taken, or the test was simply incorrect. When I had the opportunity to be tested for antibodies specific against COVID19, I had myself tested.

performed by Dr. Minguita Padilla
Thanks to Dr. Minguita Padilla who had access to test kits and graciously performed the rapid antibody test on me. I turned IgG positive, implying that as I had suspected, I indeed had a prior COVID19 infection. [IgG is short for immunoglobulin-G, antibodies that form after you have recovered from an infection in the past].
Processing
I had mixed emotions. I felt fear: I could have turned for the worse too. I was not ready. My son was not ready. Is anyone really ready? There was relief, somehow, I survived the ordeal and now have antibodies to fight the disease. Then there was this deep sense of responsibility: if my antibodies will help someone get well, I needed to donate my plasma.
Donating Plasma

I was initially rejected as a donor. Most centers doing plasmapheresis required a positive RT-PCR test, that will turn negative at least twice. I only had an RT-PCR test done once, that turned out negative and did not meet the usual criteria. I nagged Dr. Karl to give me my results from the Destura test kit, maybe that turned out positive. I was initially “rejected” too at the University of the Philippines-Philippine General Hospital, being the first potential donor that did not have an RT-PCR test that was positive. I told them about the parallel testing on the UP-NIH test kit for validation, and hope they could gain access to it.
It was Dr. Jonas del Rosario who rechecked parameters for donation. There was a third parameter –a “positive result for anti-SARS-CoV-2 IgG antibody-based test done on recovery.” Yey! I absolved Dr. Karl, God bless him for all the work he does, he needed a break from me!
After at least 28 days of no symptoms, on April 20, 2020, I finally donated convalescent plasma (that yellow-orange fluid component you see inside the bag) at the University of the Philippines College of Medicine, Paz Mendoza Building Room 108 in the hope that it can help someone fighting COVID19 who was not as lucky as I was. Room 108 brought back all good memories…I was a student again of health informatics in this room at fifty. I learned new skills here. This time, however, the feeling was even better. I can donate every two weeks, at most twelve times in a year, God-willing I hope I can fulfill that responsibility.
Why donate?
I could not be at the frontlines. This was the only way I could think of to give back. I owe it to all of you staying in your houses, to all of you donating and finding ways to help our frontliners, frontliners on the streets, residents, fellows, teachers, mentors and colleagues, and other health care workers at the hospital frontlines, some of whom had paid dearly for this with their own lives.
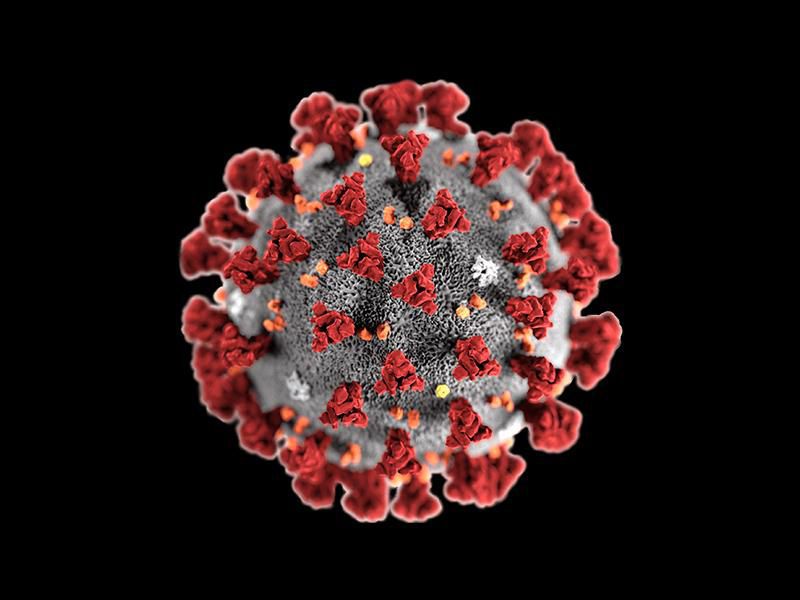
SARS-CoV2, the virus responsible for COVID19 will be beaten. The heart and soul of mankind will win. Our task is daunting, but #WeHealasONE and #WeWinasOne.